Exercise and OA
A combination of physical activity and patient education should be the first-line treatment for osteoarthritis, regardless of disease stage.
Exercise is the best treatment for people with osteoarthritis (OA) as it has the same analgesic effect as painkillers but without side effects. When we exercise, our brain releases endorphins, a hormone that works as the body’s natural painkillers. Exercise also strengthens the muscles and improves muscle coordination, which stabilizes the joints, thus reducing joint pain. Patient education is also an important part of OA first-line treatment as knowledge leads to an increased understanding of the disease and what treatment methods are available.
Being physically active is not only important for treating OA symptoms but also for general health and preventing comorbidities such as diabetes, cardiovascular diseases, and depression. The World Health Organization (WHO) recommends around 2.5 hours of exercise a week to improve or maintain good health.
Exercise is important, not only for osteoarthritis
There is a common myth that exercise wears out the joints and that people with OA should be cautious of exercising. This is not true, and it is in fact the opposite; our bodies are made to move, and exercise keeps our joints healthy. OA is not a “wear and tear” disease as was once believed. Today we know that several factors play a role in the development of the disease, such as aging, genes, previous joint injuries, and a sedentary lifestyle. Not being physically active enough can in fact contribute to weak muscles, stiff joints, and joint pain. Lack of physical activity is also linked to an increased prevalence of obesity, a major risk factor for OA.
Unfortunately, most people living with OA do not meet the recommended guidelines for physical activity. Reasons could for example be that they aren’t used to exercising or they have reduced their amount of exercise as a result of being diagnosed with OA or other medical issues.
Individualized training
Since everyone has a different experience with exercise, in terms of how much they exercise or how able they are to exercise, it is important to adjust your exercise regime based on your ability, needs, and goals. If you have recently been diagnosed with OA, it could be a good idea to start off exercising with the help of a physiotherapist (an occupational therapist can help with hand OA exercises) who can provide you with an individualized training program (supervised or unsupervised). These individualized exercises should be performed 2-3 times a week for at least 6-8 weeks to improve OA symptoms. After these weeks, you may choose to either continue with your individualized training program or switch to some form of aerobic or strength training. What is most important is that you continue being physically active. If you aren’t used to exercising or you suffer from a lot of pain, you can shorten your training sessions, but do them more often. As you get used to exercising and your joint pain improves, you may increase the length of the sessions gradually. The body gets used to exercising very quickly and your overall cardiorespiratory fitness and strength improve for each time you exercise. Short and frequent exercise sessions are better for the joints than long and infrequent sessions.
Great for the body and mind
Regular exercise has been shown to improve joint mobility and reduce pain as well as improve balance, cardiorespiratory fitness, muscle strength, and overall physical and mental health. Most people generally feel better after being physically active. The proven benefits of exercise on both physical and mental health are good enough reasons to keep exercising whether you experience pain relief or not.
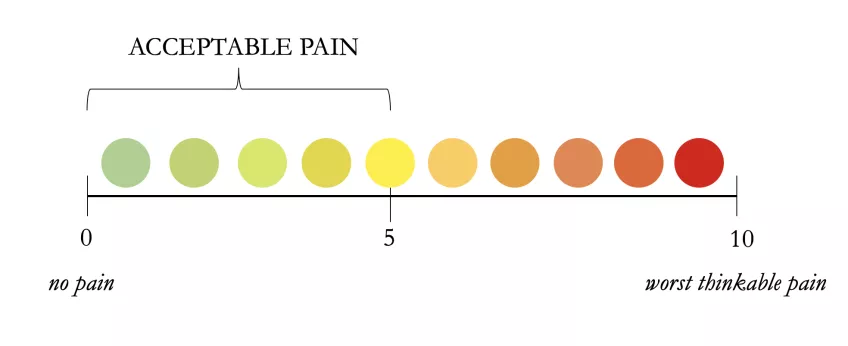
The 24-hour rule
People with OA sometimes feel discouraged about exercising when experiencing pain during or immediately after a workout session. This may result in not exercising at all which can worsen OA symptoms over time. It is totally normal to experience a certain degree of joint pain when exercising. If this happens, there is no need to worry, neither is there any need to stop exercising. As long as the pain you experience during your exercise session has returned to its "normal state" within 24 hours, you can continue with the same type of exercise. However, if the pain doesn’t get better after 24 hours, or it gets worse, you will need to adjust your exercise routine by either exercising less intensely or choosing another type of exercise.
Lifelong treatment
For most people living with OA, it is crucial to exercise to live an active life with manageable or no symptoms. This also applies to those who need or who have undergone joint replacement surgery. Physical activity is just as important before as after surgery. Being physically active should be considered a lifelong treatment for OA as exercising occasionally isn’t enough to manage symptoms long-term. For exercise to have a lasting positive effect on joint pain, it should be woven into your everyday life. Doing some form of exercise that you actually enjoy, increases the chances of being consistent with your workout routine.
Exercising together with others can increase motivation if this is lacking. Group training or brisk walks with friends are good options for those who hate exercising alone.
The World Health Organization (WHO) recommends 150-300 minutes of moderate-intensity or 75-150 minutes of high-intensity aerobic physical activity per week. These minutes can be divided into different exercise sessions throughout the week, but each session should be at least 10 minutes long. Examples of aerobic physical activity include swimming, cycling, Nordic walking, and speed walking.
If you are unable to achieve the recommendations for aerobic physical activity due to reduced mobility, severe pain, or other reasons, try to be as physically active as you can.